The Importance of Ergonomics In Dentistry

This article was originally published on Decisions in Dentistry. Written by Juan Carlos Ortiz Hugues, DDS, CEAS, an Endodontist practicing in Panama. He is a Global microscope user and has recently published “Ergonomics Applied to Dental Practice” published by Quintessence. He lectures globally on ergonomics using a microscope.
An exploration of various aspects of ergonomic practice that, if managed properly, can create an efficient working environment that promotes wellness among dental team members.
Reports indicate that 33% to 87% of dentists experience musculoskeletal pain and/or musculoskeletal disorders (MSDs) in their back, neck and shoulders.1,2 The high prevalence of MSDs among dental practitioners suggests the need for a greater focus on the practice of dental ergonomics, as this problem begins in dental school. In fact, research by Rising et al3 shows that 70% of dental students experience back pain by their third year of training.
Ergonomics is an applied multidisciplinary science that studies people’s efficiency in their working environment. It aims to increase safety and efficiency by optimizing the interaction between individuals and the tools and materials they use in their daily work. Beyond the physical aspects, however, there are mental considerations, as a truly ergonomic practice environment will not only support musculoskeletal health — it can also promote mental health by minimizing stress and fatigue.
The best approach, of course, is to prevent MSDs, because if not addressed in a timely manner these disorders can progress to serious illness — even to the point of permanent disability.4 Fortunately, these painful and potentially debilitating work-related injuries can be prevented. The key is to (1) address and optimize the body’s biomechanics during daily tasks, (2) use a teamwork approach with the appropriate technology, and (3) employ basic organizational techniques to minimize risk factors in clinical practice.5
FOUR FACTORS TO MANAGE
This article will explore the various considerations involved in ergonomic practice, including personal, organizational, financial and physical factors that, if managed properly, can help create an efficient working environment with minimal stress.
Personal Factors — Age, gender and hereditary traits are individual factors that impact operator performance and burnout susceptibility. In terms of preventing MSDs, maintaining physical fitness has been shown to help the body fatigue less rapidly and recover faster. In addition, personal habits — including sleep deprivation, substance abuse and smoking — can be significant problems affecting worker performance, especially in high-demand jobs and those with long duty periods.6–8
Mitigation strategies include practicing healthy habits outside of work, such as ensuring adequate sleep and exercising regularly to improve stamina.
Organizational Factors — Macroergonomics, a wing of the human factors and ergonomics sciences, plays an important role as it addresses the organizational and sociotechnical context of work processes. It aims to improve teamwork and organization, while also promoting efficiency within daily tasks — all of which helps support better treatment outcomes.9,10
Dental practice places multifactorial demands on clinicians due to the degree of precision involved in clinical care. In addition to time pressure, managing patient anxiety and a large armamentarium of instruments, equipment and materials creates a stressful environment — especially for practice owners.
These factors, which by necessity involve high cognitive demands, increase providers’ risk for MSDs and burnout, and thus must be properly managed to facilitate adequate performance and reduce physical and mental fatigue.11,12 Similarly, creating an ergonomic practice environment plays a crucial role in preventing psychological disorders related to depression and emotional exhaustion — risks that have been exacerbated as a result of the COVID-19 pandemic.13
An efficient way to control the cognitive stress that triggers physical stress is to organize the work according to type of task, working time per activity, and work-rest cycles.14 Among other considerations, it helps to preorganize the items to be used — a tactic that will increase efficiencies and help dental teams achieve an optimal physical/mental balance in the workplace.
Financial Factors — Educational debt and financial issues related to the procurement of the practice, continuing education, and the addition of dental technologies can lead to stress that contributes to dentists’ risk for MSDs.15,16 The physical and emotional demands of providing care in a safe environment while running a business also elevate the clinician’s risk level.
Another economic consideration is that loss of working days and physician or chiropractic visits related to MSDs will reduce clinical productivity,17 resulting in economic losses. Coupled with somatic discomfort, these concerns can compromise quality of life for dentists and auxiliaries.18 Additionally, such stress results in reduced efficiency — and possibly also quality of care due to a loss of strength and inability to focus.19
Besides postural awareness and stretching regularly, the implementation of effective office organization and administrative strategies can help mitigate stress-related MSDs.

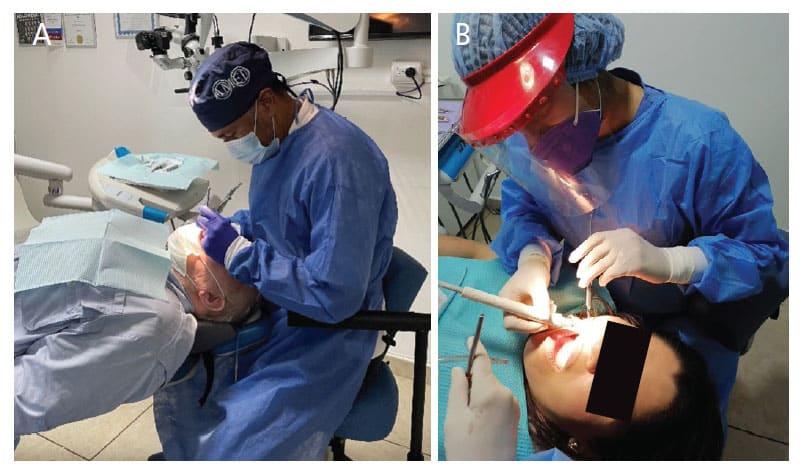
Physical Factors — The high prevalence of MSDs in dentistry closely relate to the following physical risk factors (Figures 1A and 1B):
- Awkward postures
- Repetition of tasks and movements
- Force
- Duration of the task (e.g., more than two hours)
- Higher degrees of flexion, particularly flexion exceeding 45°
Trunk flexion angles greater than 20° forward are considered awkward.20 Additionally, axial rotation along with flexion and lateral flexion contribute to the varied combination of risk factors for MSDs.21,22
Ultimately, it is much more efficient to start young dentists off with excellent ergonomic habits than attempt to correct them in the future; thus, practice ergonomics should be included in school curricula. Fortunately, MSDs can be prevented by utilizing preventive measures, which include specially designed equipment, such as ergonomic stools, loupes, surgical microscopes, endoscopes and other visual aids, and operatory-specific mobiliary.23
The prevalence of low back and/or neck pain in dentists reportedly ranges between 13% to 89%.24 It has been shown that postures that exert higher pressure on intervertebral disks and prolonged spinal hypomobility are important risk factors leading to degenerative changes in the lower back and cervical spine. There is a strong relationship between static muscle contractions and muscle ischemia/necrosis due to static posture.25 Even so, many dentists continue working despite a decline in their physical condition, which has the potential to put patients’ health at risk.26 And, not surprisingly, MSDs have been reported as the most frequent cause of early retirement.27
One of the factors that generate a physiologically negative practice environment is a prolonged static posture. Stretching and regular breaks promote increased blood flow that removes waste products from the muscles. There is evidence that stretching decreases musculoskeletal pain in dental professionals, while a lack of regular weekly exercise correlates with increased lower back pain.28,29
OPERATOR/PATIENT POSITIONING
Working at the 12 o’clock position (behind the patient’s head) places the operator in the most neutral working posture, which is also improved by placing the patient in the most horizontal position in the chair.30 A reference point is to place the mouth of the patient at the height of the dentist’s elbows, with the patient’s head at the end of the headrest. Clinicians should then use verbal cues for the strategic view angulation of the oral cavity without disturbing the operator’s head posture.
Guidelines for a neutral sitting posture, which results in a biomechanical advantage and reduced stress to the musculoskeletal system (Figure 2) include keeping or maintaining:31
- An erect or upright spine
- Hands, wrists, and forearms straight, in-line, and parallel to the floor
- Elbows relaxed at both sides of the body, with no more than 10° of abduction, and forearms parallel to the floor or slightly upward to 10°
- The head and neck in an upright position (ears over shoulders, shoulders over hips) and aligned with the torso
- Hips higher than the knees in a seated posture
- The back fully supported, using appropriate lumbar support
Each team member must understand the body’s biomechanics, especially sitting posture. It has been shown that clinicians who receive postural feedback and recommendations improved their neck and upper back extensions during subsequent operatory tasks.32
When using four-handed dentistry, a well-trained dental assistant should handle and transfer instruments and equipment that have been strategically placed at short horizontal-reach distances of between 14 and 25 inches. This positioning allows efficient transfers to the operator. The teamwork afforded by a four-handed technique encourages proper working posture among both clinicians, while reducing unnecessary movements.33

ERGONOMIC OFFICE DESIGN AND TOOLS
In ergonomic practice, office design and layout should focus on efficient workflows and the health of the entire dental team. Similarly, the selection of furniture and equipment should support these efficiencies — especially a coordinated workflow between the dentist and dental assistant.34
Proper equipment selection has been shown to significantly mitigate musculoskeletal issues and symptoms in the dental setting. This includes the choice of mobiliary and ergonomic operator stools (Figure 3), and the use of dental mirrors and magnification aids, such as loupes and the surgical microscope.35,36
When working without magnification, the dentist compensates for the lack of visual acuity by moving the eyes closer to the patient’s mouth, resulting in cervical and lumbar stress due to the flattening of the lumbar and/or cervical curves caused by the forward-leaning posture.37
Dentist and dental assistant stools should provide lumbar support, with an appropriate convex shape and dimension adjusted according to individual body anthropometrics. Additionally, the seat should be adjustable in its inclination to promote a hip angle that is higher than the knees. Stools with arm and elbow support can also prove beneficial, especially those that allow adjustments in height and width to help optimize support of upper limbs, which can reduce muscle fatigue in the median neck and shoulders.38
BENEFITS OF MAGNIFICATION
Using loupes or microscopes has been shown to improve clinicians’ working posture and reduce repetitive stress injuries related to ergonomically inefficient posture and practice.39,40 Loupe selection should be based on the clinician’s musculoskeletal and clinical needs and address factors such optimal positioning, working distance, and the loupes’ declination angle and depth of field.41
The synergy between an ergonomically designed stool and use of loupes or other aids, such as the surgical microscope or dental endoscope, facilitates a more ideal working posture than when using less optimal stools and no magnification.42 In practice, this increased visual acuity helps support better care and improved outcomes. In addition, the surgical microscope’s multiple magnification settings and coaxial lighting on the visual axis — which does not cast shadows in the working field — further promote efficient and effective care. Proper lighting is particularly helpful, since by increasing light levels clinicians can simultaneously increase apparent resolution.43 Designed to improve direct and indirect vision,44 the microscope allows operators to adopt a neutral working posture (provided the necessary adjustments and positioning are rigorously followed). With daily use, however, clinical practice with the microscope becomes a routine part of care (Figure 4).

SUMMARY
Adopting ergonomic equipment and working posture — as well as ensuring a carefully organized operatory layout — can help oral health professionals avoid MSDs that could potentially compromise career longevity. Toward that goal, the following list sums up seven key points to consider:
- The human body is not designed biomechanically, anatomically or physiologically to work long hours while sitting.
- Visual requirements in dental care often compromise working posture; thus, use of magnification and coaxial lighting is recommended.
- Thoughtful organization of the operatory environment aids ergonomic practice.
- In terms of the clinical team, programmed stretching and regular breaks are crucial to the mental and physical health of the dentist and staff.
- The use of operating microscopes and ergonomic stools (as well as stool adjustment techniques) should be taught in dental school.
- With proper training, the dental assistant’s participation improves workflows, as well as the efficiency and care provided by the dentist.
- The systematized positioning of the operator, patient, and assistant will support optimal biomechanics during the provision of care.
In closing, and as noted at the outset, the benefits of ergonomic practice extend beyond the physical demands of treatment — because offices that embrace these principles will also promote mental health and wellness by minimizing stress and fatigue.
REFERENCES
- Marshall ED, Duncombe LM, Robinson RQ, Kilbreath SL. Musculoskeletal symptoms in New South Wales dentists. Aust Dent J. 1997;42:240–246.
- Ohlendorf D, Naser A, Hass Y, et al. Prevalence of musculoskeletal disorders among dentists and dental students in Germany. Int J Environ Res Public Health. 2020;17:8740.
- Rising DW, Bennett BC, Hursh K, Plesh O. Reports of body pain in a dental student population. J Am Dent Assoc. 2005;136:81–86.
- Alexopoulos EC, Stathi IC, Charizani F. Prevalence of musculoskeletal disorders in dentists. BMC Musculoskelet Disord. 2004;5:16.
- Anshasi RJ, Alsyouf A, Alhazmi FN, AbuZaitoun AT. A change management approach to promoting and endorsing ergonomics within a dental setting. Int J Environ Res Public Health. 2022;19:13193.
- Knapik J. The importance of physical fitness for injury prevention: part 1. J Spec Oper Med. 2015;15:123–127.
- Antoniadou M. Estimation of factors affecting burnout in Greek dentists before and during the COVID-19 pandemic. Dent J. 2022;10:108.
- Laborde S, Kauschke D, Hosang TJ, Javelle F, Mosley E. Performance habits: a framework proposal. Front Psychol. 2020;11:1815.
- Ross A. Human factors and ergonomics for the dental profession. Dent Update. 2016;43:688–690, 692–695.
- Carayon P, Karsh BT, Gurses AP, et al. Macroergonomics in healthcare quality and patient safety. Rev Hum Factors Ergon. 2013;8:4–54.
- Marcora SM, Staiano W, Manning V. Mental fatigue impairs physical performance in humans. J Appl Physiol. 2009;106:857–864.
- Hakim H, Khemiri A, Chortane OG, et al. Mental fatigue effects on the produced perception of effort and its impact on subsequent physical performances. Int J Environ Res Public Health. 2022;19:10973.
- Owen C, Seddon C, Clarke K, Bysouth T, Johnson D. The impact of the COVID-19 pandemic on the mental health of dentists in Wales. Br Dent J. 2022;232:44–54.
- Naidoo S. Managing stress in the dental environment. S Afr Dent J. 2015;70:n.9.
- Rada RE, Johnson-Leong C. Stress, burnout, anxiety and depression among dentists. J Am Dent Assoc. 2004;135:788–794.
- Jena M, Satyarup D, Nagarajappa R, Dhar U. Stress in dentistry: a review. Indian J Forensic Med Toxicology. 2021;14:8667–8670.
- Yamalik N. Musculoskeletal disorders (MSDs) and dental practice part 2. Risk factors for dentistry, magnitude of the problem, prevention, and dental ergonomics. Int Dent J. 2007;57:45–54.
- Antonopoulou MD, Alegakis AK, Hadjipavlou AG, Lionis CD. Studying the association between musculoskeletal disorders, quality of life and mental health. A primary care pilot study in rural Crete, Greece. BMC Musculoskelet Disord. 2009;10:143.
- Lalumandier JA, McPhee SD. Prevalence and risk factors of hand problems and carpal tunnel syndrome among dental hygienists. J Dent Hyg. 2001;75:130–134.
- Nourollahi M, Afshari D, Dianat I. Awkward trunk postures and their relationship with low back pain in hospital nurses. Work. 2018;59:317–323.
- McGill SM, Grenier S, Kavcic N, Cholewicki J. Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol. 2003;13:353–359.
- U.S. Centers for Disease Control and Prevention. Musculoskeletal Disorders and Workplace Factors. Available at: https://www.cdc.gov/niosh/docs/蒭-141/pdfs/蒭-141.pdf?id=10.26616/NIOSHPUB97141. Accessed December 9, 2022.
- Motghare V, Singh M. Ergonomics in dentistry: Narrative review. Int J Appl Dent Sci. 2018;4:104–110.
- Al Otaibi F, Nayfeh FM, Alhussein JI, Alturki NA, Alfawzan AA. Evidence based analysis on neck and low back pain among dental practitioners — A systematic review. J Pharm Bioallied Sci. 2022;14(Suppl S1):S897–S902.
- Alipour A. Neck and shoulder pain: prevalence, incidence and risk factors, the IKCo cohort study. Available at: https://openarchive.ki.se/xmlui/handle//屩. Accessed December 9, 2022.
- Puriene A, Janulyte V, Musteikyte M, Bendinskaite R. General health of dentists. Literature review. Stomatologija. 2007;9:10–20.
- Murphy DC. Ergonomics and dentistry. NY State Dent J. 1997;63:30–34.
- Roll SC, Tung KD, Chang H, et al. Prevention and rehabilitation of musculoskeletal disorders in dental professionals: A systematic review. J Am Dent Assoc. 2019;150:489–502.
- Shariat A, Cleland JA, Danaee M, Kargarfard M, Sangelaji B, Tamrin SBM. Effects of stretching exercise training and ergonomic modifications on musculoskeletal discomforts of office workers: a randomized controlled trial. Braz J Phys Ther. 2018; 22:144–153.
- Blanc D, Farre P, Hamel O. Variability of musculoskeletal strain on dentists: an electromyographic and goniometric study. Int J Occup Saf Ergon. 2014;20:295–307.
- Valachi B. Practice Dentistry Pain-Free. Evidence-Based Strategies to Prevent Pain and Extend Your Career. Portland, Ore: Posturedontic Press; 2008:26–27.
- Thanathornwong B, Suebnukarn S. The improvement of dental posture using personalized biofeedback. Stud Health Technol Inform. 2015;216:756–760.
- Singh N, Jain A, Sinha N, Chauhan A, Rehman R. Application of four-handed dentistry in clinical practice: A Review. Int J Dent Med Res. 2014;1:8–13.
- Hokwerda O, Wouters JA, de Ruijter RA, Zijlstra-Shaw S. Ergonomic requirements for dental equipment. Guidelines and recommendations for designing, constructing and selecting dental equipment. Available at: https://esde.org/files/publication/葚-ergonomic_requirements_for_dentalequipment._april2007.pdf. Accessed December 9, 2022.
- Saxena P, Gupta SK, Jain S, Jain D. Work-related musculoskeletal pain among dentists in Madhya Pradesh, India: prevalence, associated risk factors, and preventive measures. Asia Pac J Public Health. 2014;26:304–309.
- García-Vidal JA, Lopez-Nicolas M, Sanchez-Sobrado AC, Escolar-Reina MP, Medina-Mirapeix F, Bernabeu-Mora R. The combination of different ergonomic supports during dental procedures reduces the muscle activity of the neck and shoulder. J Clin Med. 2019;8:1230.
- Katano K, Nakajima K, Saito M, Kawano Y, Takeda T, Fukuda K. Effects of line of vision on posture, muscle activity and sitting balance during tooth preparation. Int Dent J. 2021;71:399–406.
- Bolderman FW, Boz-Huizer JA, Hoozemans MJ. The effect of arm supports on muscle activity, posture, and discomfort in the neck and shoulder in microscopic dentistry: Results of a pilot study. IISE Trans Occup Ergon Hum Factors. 2017;5:1–14.
- Del Fabbro M, Taschieri S, Lodi G, Banfi G, Weinstein RL. Magnification devices for endodontic therapy. Cochrane Database Syst Rev. 2015;12:CD005969.
- Belcher JM. A perspective on periodontal microsurgery. Int J Periodontics Restorative Dent. 2001;21:191–196.
- Mansueto MA, Overton JD. A clinician’s guide to purchasing surgical loupes. Tex Dent J. 2007;124:174–186.
- Dable RA, Wasnik PB, Yeshwante BJ, Musani SI, Patil AK, Nagmode SN. Postural assessment of students evaluating the need of ergonomic seat and magnification in dentistry. J Indian Prosthodont Soc. 2014;14(Suppl 1):51–58.
- Carr GB, Murgel CAF. The use of the operating microscope in endodontics. Dent Clin N Am. 2010;54:191–214.
- Eichenberger M, Biner N, Amato M, Lussi A, Perrin P. Effect of magnification on the precision of tooth preparation in dentistry. Oper Dent. 2018;43:501–507.
From Decisions in Dentistry. January 2023;9(1)34-36,39.


.png)